Assessment and Biomarkers
Assessment
Breast cancer evaluation should be an ordered inquiry that starts with symptoms, comprehensive clinical history, and evaluation of risk factors. This is followed by a sequence that has become formalized as triple assessment1:
- Clinical examination
- Imaging (usually mammography, ultrasonography, or both)
- Needle biopsy
The foundation for the diagnosis of breast cancer remains standard pathomorphological diagnostics.2 Histopathological examination should include:
- Histological type of the tumor
- The degree of histological malignancy
- The degree of advancement according to the tumor, node, metastasis (TNM) classification
- Information on the completeness of the procedure
- Infiltration by cancer cells of peritugal vessels
- Expression of steroid receptors (estrogen and progesterone), HER-2 receptor, and cellular proliferation index Ki673
Assessment of the above parameters is possible based on a coarse needle biopsy or intraoperative and postoperative material.4 The correct protocol of histopathological examination, considering the biological subtype of the tumor, determines predictive and prognostic factors as well as subsequent selection of appropriate, individualized treatment.5
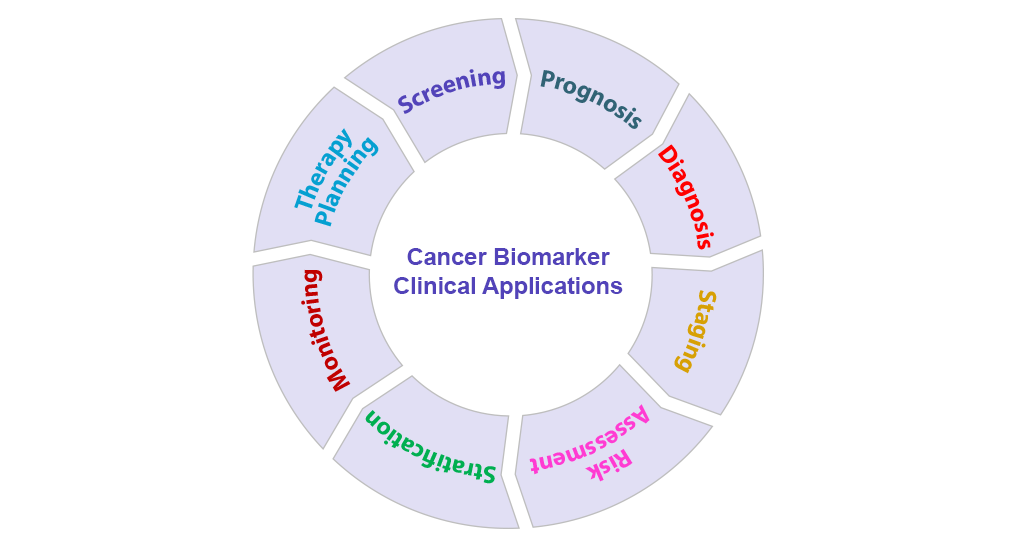
Biomarkers
As breast cancer is a heterogeneous disease, biomarkers are used to determine the treatment strategy. As a result it is critical that clinicians test patients to establish tumor characteristics.6 Identification of mutations that confer resistance to endocrine therapy can help clinicians select the most beneficial treatment for patients with ER+ metastatic breast cancer. Resistance can develop through several mechanisms; however, the most common are mutations in the ESR1 gene that fixes the ER in an active conformation and mutations that activate the PI3K/AKT/mTOR pathway.7
The most common biomarkers for breast cancer are hormone receptor and HER2 status, as discussed elsewhere on this website. However, other biomarker tests are used for certain tumors. These include:
- PD-L1 status
- Genomic testing
- ESR1, PIK3CA, BRCA1, and BRCA2 mutation status
- Tumor mutation burden
- Ki-67, CA 27-29, CA 125, and CEA levels
- Broad molecular profiling
- Circulating tumor DNA (ctDNA) assessment
Fortunately, liquid biopsy techniques are emerging for testing such biomarkers and may also offer the benefit of monitoring tumor dynamics over time.6 These can be used for the diagnosis, prognosis, and monitoring of treatment response through the detection of ctDNA. ctDNA is released into the blood stream through tumor cell necrosis or apoptosis and is particularly useful for detection, monitoring treatment response, and longitudinal sampling. Liquid biopsy for ctDNA analysis is recommended for biomarkers such as ESR1, and ctDNA analysis of liquid biopsy samples can provide real-time data describing tumor dynamics and genetic alterations.6,8 This is important for ESR1 as retesting of initial wild-type samples is recommended at disease progression.6,8
References
- Chalasani P. Breast cancer workup. https://emedicine.medscape.com/article/1947145-workup.
- Leong AS, Zhuang Z. The changing role of pathology in breast cancer diagnosis and treatment. Pathobiology. 2011;78:99-114.
- Makki J. Diversity of breast carcinoma: histological subtypes and clinical relevance. Clin Med Insights Pathol. 2015;8:23-31.
- Rakha EA, Ellis IO. An overview of assessment of prognostic and predictive factors in breast cancer needle core biopsy specimens. J Clin Pathol. 2007;60:1300-1306.
- Smolarz B, Nowak AZ, Romanowicz H. Breast cancer: epidemiology, classification, pathogenesis and treatment (review of literature). Cancers (Basel). 2022;14(10):2569.
- Venetis K, Cursano G, Pescia C, et al. Liquid biopsy: cell-free DNA based analysis in breast cancer. J Liquid Biopsy. 2023;1:100002.
- Neupane N, Bawek S, Gurusinghe S, et al. Oral SERD, a novel endocrine therapy for estrogen receptor-positive breast cancer. Cancers. 2024;16:619.
- Burstein HJ, DeMichele A, Somerfield MR, Henry NL. Testing for ESR1 mutations to guide therapy for hormone receptor–positive, human epidermal growth factor receptor 2–negative metastatic breast cancer: ASCO guideline rapid recommendation update.
J Clin Oncol. 2023;41:3423-3425.